Insulin Glulisine
About Insulin Glulisine
Insulin Glulisine used for the treatment of both type 1 and type 2 diabetes mellitus. In Type 1 diabetes mellitus, the body does not produce enough insulin to regulate blood sugar levels. In type 2 diabetes mellitus, either the body stops producing enough insulin (a hormone that helps lower blood sugar levels) or there is resistance to the action of insulin. As a result, insulin is produced in large quantities, but it is unable to function correctly in the body's organs.
Insulin Glulisine contains insulin glulisine, which helps normalize blood sugar levels by facilitating the movement of sugar from the blood into other tissues of the body. It reduces the risk of severe diabetes complications. It stimulates the recovery of sugar in muscle and fat cells, thereby suppressing the production of sugar in the liver.
Not everyone who is taking Insulin Glulisine will get these side effects. You may experience rash, injection site allergic reaction, weight gain, edema (tissue swelling or fluid overload), skin thickening at the injection site, low blood glucose levels, and itching. Most of these side effects of Insulin Glulisine do not require medical attention and typically resolve on their own over time. However, if the side effects are persistent, reach out to your doctor.
Insulin Glulisine should be taken before food or advised by your doctor. It should be administered subcutaneously (in the upper thigh, abdomen, upper arm, or buttocks) only. Your doctor will explain how to administer the medicine yourself. However, if it is difficult to inject the medicine, ask a healthcare professional to take it. Along with Insulin Glulisine, you should maintain a healthy diet, engage in regular exercise, and adhere to your doctor's weight management advice.
Inform your doctor if you are allergic to Insulin Glulisine. Do not take Insulin Glulisine if you have any low blood glucose levels, kidney, liver, or heart problems, or problems with alcohol or other prescription or recreational drugs. Try not to stop receiving Insulin Glulisine of your own. Let your doctor know about this, as it may cause withdrawal symptoms. Insulin Glulisine is a cold chain medicine, and so it must be stored in the refrigerator between 2-8 degrees Celsius, or else its efficiency might get lost. Do not store in the freezer or the fridge.
Uses of Insulin Glulisine
• Diabetes Management: Insulin Glulisine is primarily used to regulate blood glucose levels in individuals with diabetes mellitus, helping to keep them within a healthy range.
• Postprandial Blood Sugar Control: Insulin Glulisine effectively manages postprandial (after meal) blood sugar spikes through its combination of intermediate and short-acting insulin.
• Type 1 and Type 2 Diabetes Treatment: Insulin Glulisine is prescribed for patients with Type 1 and Type 2 diabetes who are unable to achieve adequate glycemic control with oral hypoglycemic agents alone.
Medicinal Benefits
- The primary role of insulin and insulin analogues, including insulin glulisine, is glucose metabolism control.
- Insulin lowers blood glucose levels by stimulating peripheral glucose uptake, particularly skeletal muscle and fat, and inhibiting hepatic glucose production.
- Insulin Glulisine is an antidiabetic medicine primarily used for the treatment of both type 1 and type 2 diabetes mellitus.
- It prevents the risk of having severe complications of diabetes. It stimulates the recovery of sugar in muscle and fat cells, thereby suppressing sugar production in the liver.
- Insulin Glulisine helps improve glycaemic control, which in turn decreases the risk of complications of diabetes, such as damage to the retina (retinopathy), damage to the kidneys (nephropathy), impairment of nerve cells (neuropathy), delayed wound healing, diabetic foot ulcers, and others.
- Insulin Glulisine can also be safely prescribed to the diabetic mother during pregnancy and lactation.
- It stimulates the recovery of sugar in muscle and fat cells and thus suppresses the production of sugar in the liver.
Directions for Use
- Insulin Glulisine is usually injected 15 minutes before a meal or within 20 minutes after starting a meal or as advised by your doctor.
- Follow your doctor's instructions on the dosage and timing of this medication.
- Check the label for directions and use it as advised by the doctor.
- Choose an injection site such as the thigh, upper arm, or abdomen, pinch the skin, and inject the advised dose at a 45-degree angle slowly and steadily.
- Rotate the injection site every time.
- Do not inject into skin that is red, bruised, or hard.
- Do not reuse or share needles.
Storage
Side Effects of Insulin Glulisine
- Injection site reactions (such as reddening, unusually intense pain on injection, itching, hives, swelling or inflammation)
- Hypoglycaemia (low blood sugar level)
- Hypokalaemia (low potassium)
- Lipodystrophy (fat deposition under the skin)
- Rash
- Pruritus (itchy skin)
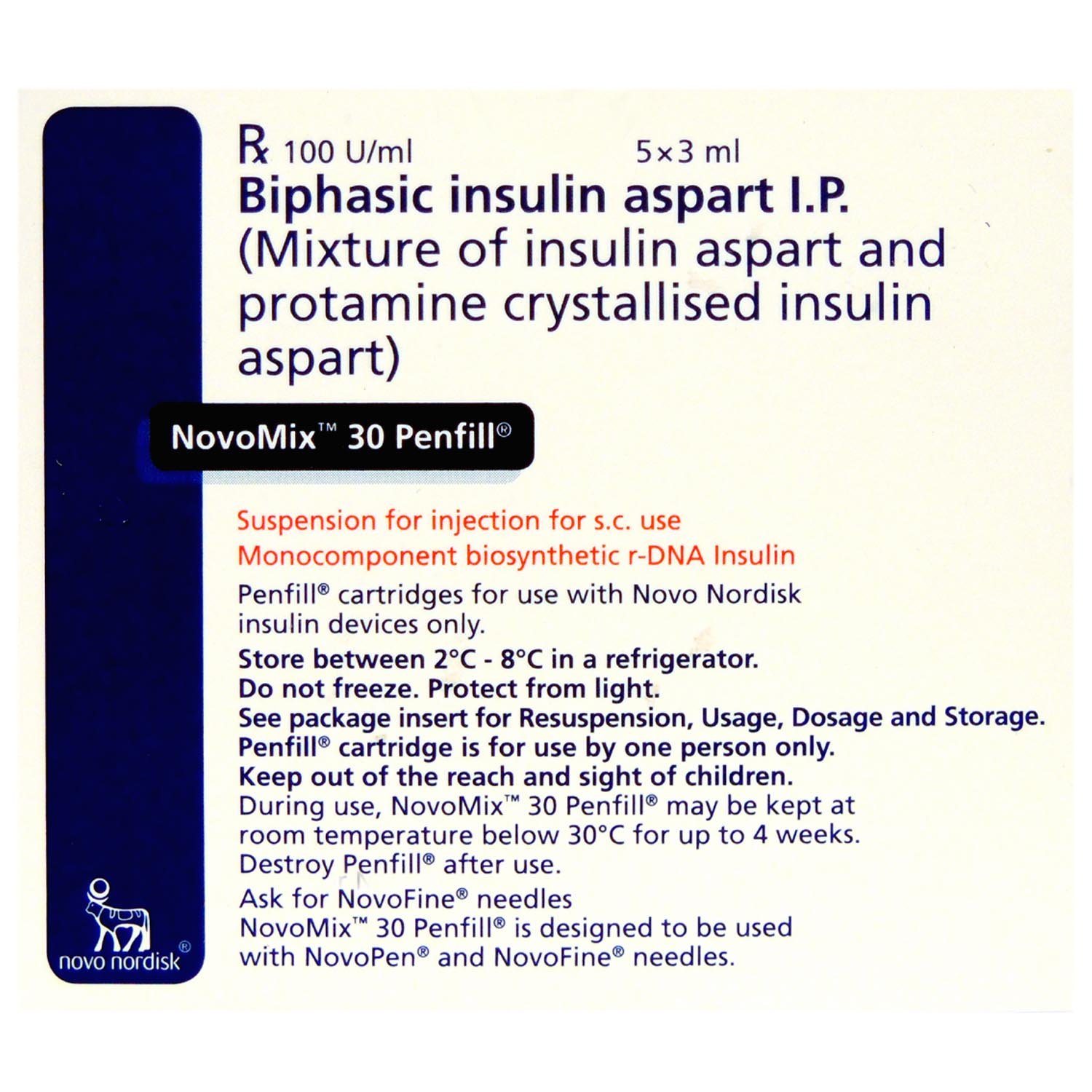
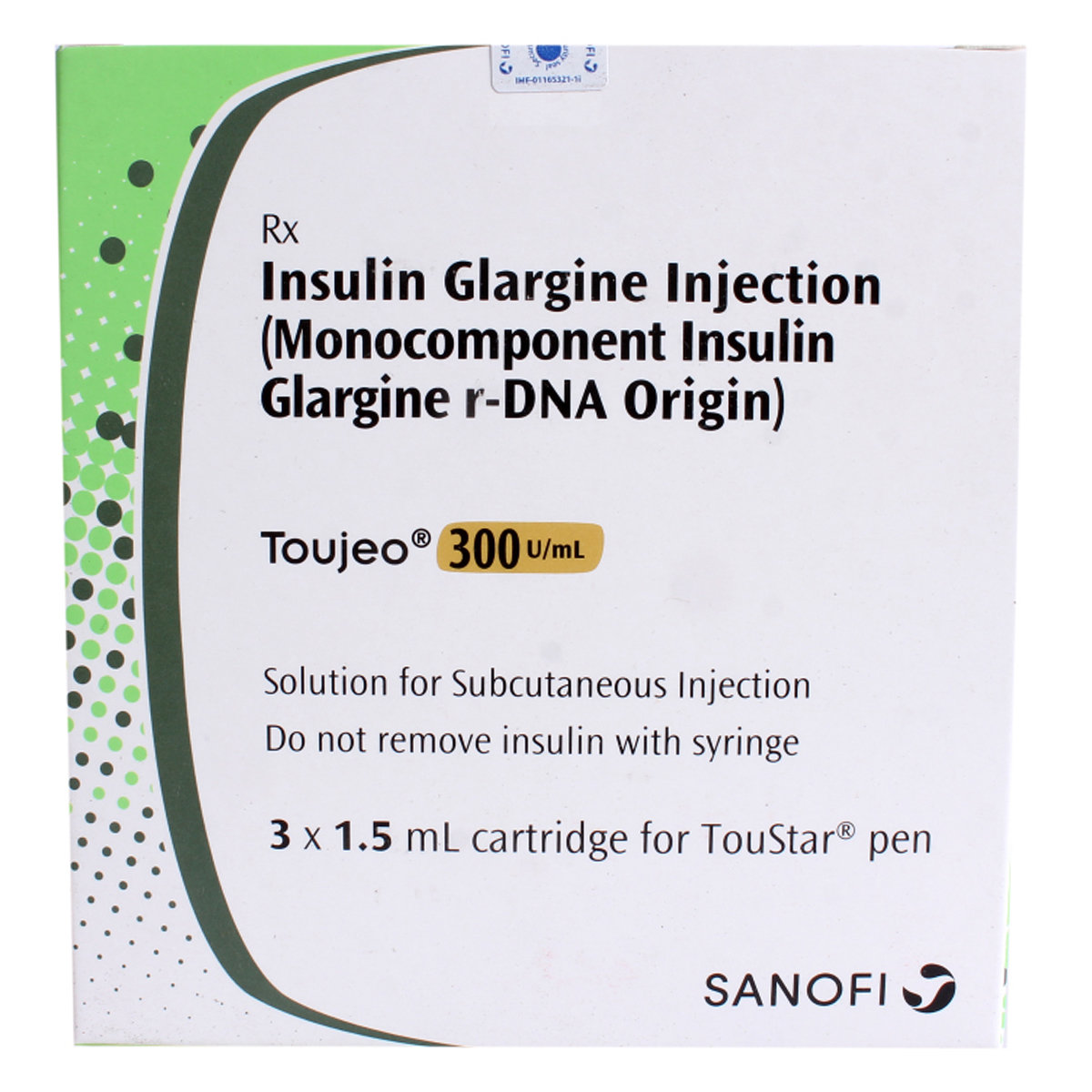
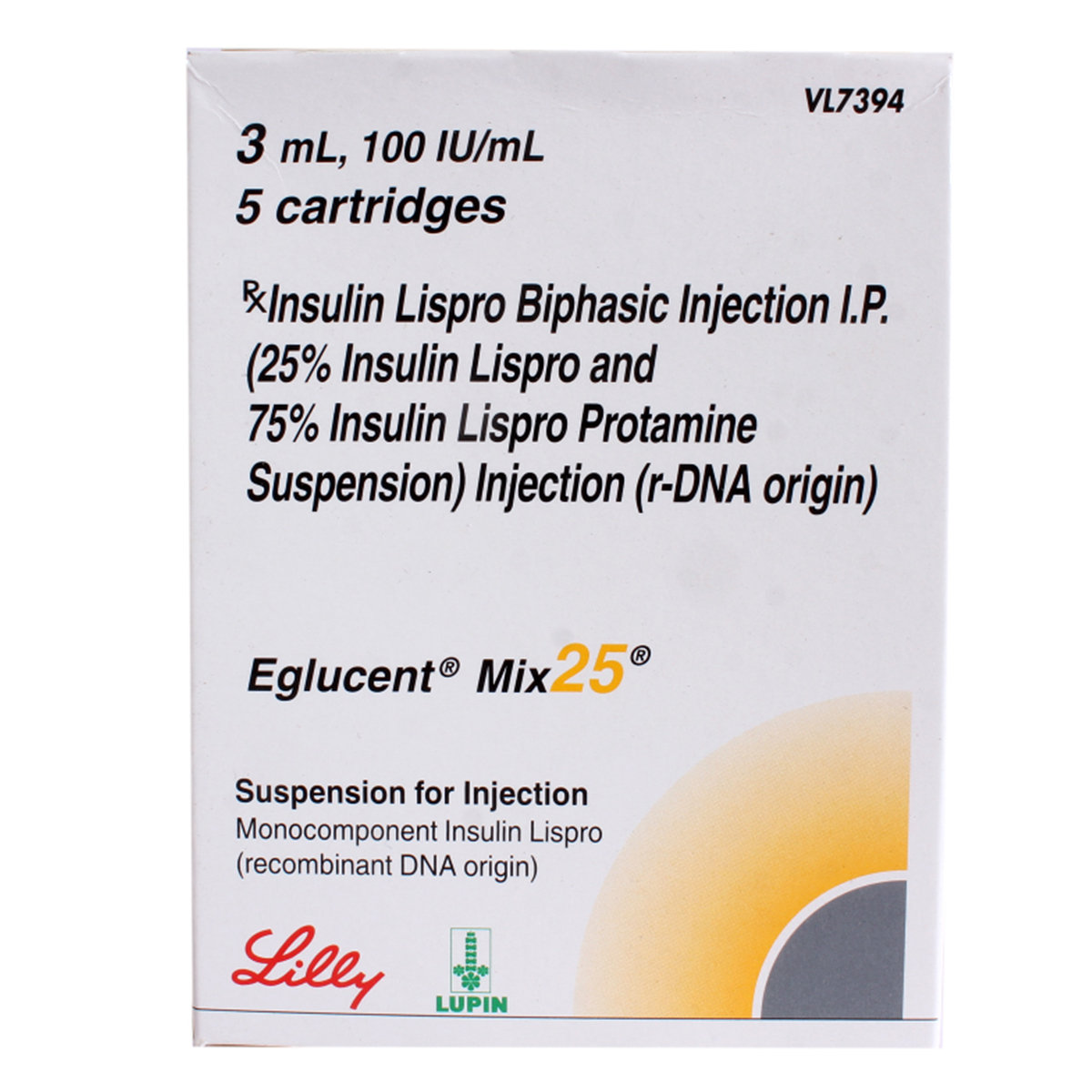
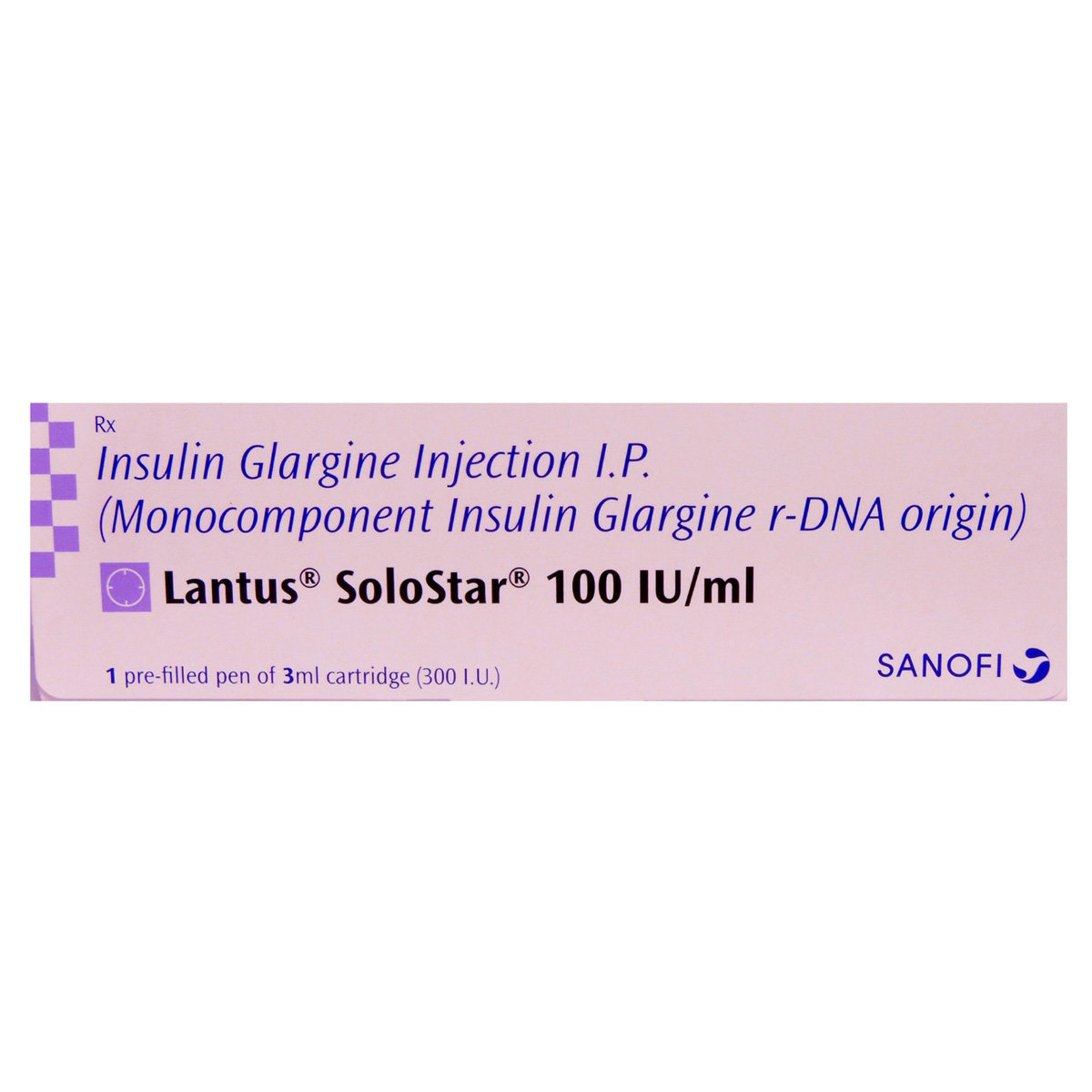
Medicines Containing this Salt
View AllDrug Warnings
- Inform your doctor if you are allergic to Insulin Glulisine. Do not take Insulin Glulisine if you have any low blood glucose levels, kidney, liver, or heart problems, or problems with alcohol or other prescription or recreational drugs.
- Try not to stop receiving Insulin Glulisine of your own. Let your doctor know about this, as it may cause withdrawal symptoms. Insulin Glulisine may decrease the level of potassium, leading to a state of hypokalaemia that, if left untreated, may lead to respiratory paralysis, irregular heartbeat rhythm, coma, and even death.
- Insulin Glulisine is for subcutaneous (under the skin) use only. If you are switching to a different insulin brand or using a different method of injection, it should be done under strict medical supervision.
- Cases of heart failure have been reported when pioglitazone was used with insulin, especially in patients at high risk of cardiac heart failure.
- The first symptoms of hyperglycemia (high blood sugar levels) may include excessive thirst, dry mouth, increased frequency of urination, nausea, vomiting, drowsiness, flushed dry skin, loss of appetite, and an acetone odour in the breath. You should closely monitor these symptoms.
- It is advisable not to consume alcohol, as it may either increase or decrease your blood glucose level.
- Care should be taken while travelling across more than two time zones. Your doctor may adjust your insulin schedule.
- Insulin Glulisine is a cold chain medicine, and therefore it must be stored in the refrigerator at a temperature between 2-8 degrees Celsius, or else its efficiency may be compromised. Do not store in the freezer or the fridge.
- Keep the medicine out of reach of children. Please do not inject more than the recommended dose of medicine, as it can cause undesirable effects.
- It is always important to check the expiry date of the medicine. Discard the medicine if it reaches the expiry date.
Drug Interactions
Drug-Drug Interactions: Insulin Glulisine may have an interaction with drugs that may increase the risk of antiarrhythmic (disopyramide), hemorheological agents (pentoxifylline), antidiabetic medicinal products (pramlintide, glucagon), beta-blockers (metoprolol), diuretics (furosemide ), bleeding disorder drugs (octreotide), antipsychotic (propoxyphene, phenothiazines), oestrogens, progestins (e.g. in oral contraceptives), protease inhibitors and atypical antipsychotic medicinal products (e.g. olanzapine and clozapine)., thyroid hormones (levothyroxine), anti-asthmatics (albuterol, epinephrine, terbutaline), antidepressant medications (fluoxetine, lithium), lipid-lowering pills (reserpine, niacin, clonidine, fenofibrate, guanethidine), pain killers (aspirin) and antibiotics (isoniazid).
Drug-Food Interactions: Insulin Glulisine may interact with an ayurvedic, homoeopathy, Unani, herbal supplements or OTC items. Tell your doctor if you are using these products. Try to avoid alcoholic beverages with Insulin Glulisine as it may increase or decrease your blood sugar level.
Drug-Disease Interaction: Insulin Glulisine should not be given to patients with kidney disease, liver disease, low blood sugar/glucose level (hypoglycaemia), and low potassium level (hypokalaemia).
Drug-Drug Interactions Checker List:
Safety Advice

Alcohol
unsafeYou are recommended not to consume alcohol along with Insulin Glulisine to avoid unpleasant side-effects. Alcohol may either decrease or increase the blood sugar level which can be fatal.

Pregnancy
safe if prescribedInsulin Glulisine can be used during pregnancy. Your insulin dose may need to be changed during pregnancy and after delivery.

Breast Feeding
safe if prescribedInsulin Glulisine can be given safely to nursing mothers but only under the supervision of a physician.

Driving
cautionDrive with caution, Insulin Glulisine usually causes drowsiness and affects driving ability. Your ability to concentrate and react may be reduced if you have hypoglycaemia (low blood sugar).

Liver
cautionInsulin Glulisine to be taken with caution, especially if you have a history of liver disease. The dose may have to be adjusted by your doctor.

Kidney
cautionInsulin Glulisine to be taken with caution, especially if you have a history of kidney disease. The dose may have to be adjusted by your doctor.

Children
safe if prescribedInsulin Glulisine can be given safely to children provided; dose has to be prescribed by a child specialist.
Habit Forming
Diet & Lifestyle Advise
- Exercise may lower your body’s need for insulin during and sometimes after physical activity.
- Exercise may also speed up the effect of an insulin dose, especially if the exercise involves the area of the injection site (for example, the leg should not be used for injection just prior to running).
- Discuss with your doctor how to adjust your insulin regimen to accommodate exercise.
- Avoid eating sugar food and prefer food cooked food low in calories.
- When travelling across more than two time zones, you should talk to your doctor concerning adjustments in your insulin schedule.
Special Advise
Your doctor may tell you to have a regular potassium level as prolonged administration causes a life-threatening condition of hypokalemia (low potassium).
Patients Concern
Disease/Condition Glossary
Diabetes: Diabetes is a chronic or lifelong disease that prevents the body from utilizing insulin properly. Insulin is the hormone that controls sugar levels in the blood. Diabetes is a condition in which blood glucose levels are above normal. It is of two types, namely: type-1 and type-2 diabetes. Type-1 diabetes is a condition in which the pancreas produces little or no insulin. Type-2 diabetes affects the way the body processes sugar. Symptoms of diabetes include lack of energy, tiredness, frequent urination, excess thirst, dry mouth, blurry vision, constant hunger, weight loss, and itchy skin.
FAQs
Insulin Glulisine is rapid-acting insulin used for the treatment of diabetes mellitus in both children (above six years of age) and adults. Insulin lowers blood glucose levels by stimulating peripheral glucose uptake, particularly skeletal muscle and fat, and inhibiting hepatic glucose production.
Insulin kept out of the refrigerator will not poison you or even make you sick. It just means that your insulin will not work as well or deliver its full potential dose. In simple terms, if your blood sugar is high, and you use the insulin that has been kept out, your blood sugar may not be lowered.
Insulin is released from the beta cells in your pancreas in response to the rise in glucose in your bloodstream. After you have consumed a meal, any carbohydrate you have eaten is broken down into glucose and transferred into the bloodstream. The pancreas detects this rise in blood glucose and starts to secrete insulin.
Habitual moderate coffee drinking has actually been associated with increased insulin sensitivity and lowered risk for type 2 diabetes. But in acute and high doses, caffeine can decrease insulin sensitivity and raise plasma insulin levels.
Insulin is released from the beta cells present in your pancreas in response to rising glucose in your bloodstream. The pancreas detects this rise in blood glucose and starts to secrete insulin.
A hard-boiled egg is a handy high-protein snack when you have diabetes. Your protein will help keep you full without impacting your blood sugar. Protein not only slows down digestion, but it also slows down the absorption of glucose. If you have diabetes, this is very beneficial.
Pramlintide, Ethanol (Alcohol) and Macimorelin have got serious interactions with Insulin Glulisine. So, do not take these medicines with Insulin Glulisine.
Insulin Glulisine can be given to treat both the condition of type 1 and type 2 diabetes mellitus. However, your doctor will decide whether Insulin Glulisine can be given to you or not, depending on your present condition. Insulin Glulisine should be avoided in patients who are allergic to Insulin Glulisine or other forms of insulin, patients with kidney disease, liver disease, low blood sugar/glucose level (hypoglycaemia), and low potassium level (hypokalaemia).
The side effects of Insulin Glulisine include injection site reactions (such as reddening, unusually intense pain on injection, itching, hives, swelling or inflammation), low blood sugar, low potassium levels, rash, itchy skin, and fat deposition under the skin. If these side effects persist or worsen, please consult your doctor.
You are recommended to avoid white bread, maida, poori, naan, noodles, biryani, fried rice, corn flakes, cheese, ice creams, milkshakes, beef, pork, sugarcane juice, soft drinks, sweetened health drinks and beverages. Also, avoid mango, seetaphal, jack fruit, fruit salads with ice cream, and fruit-based desserts.
No, do not stop taking Insulin Glulisine without consulting your doctor as it may lead to high blood sugar levels and may worsen your condition resulting in complications. If you experience any side effects or discomfort, contact your doctor. You may need dose adjustment.
Taking injection at the same site may cause local irritation, itching and lump formation. Therefore, it is best to avoid taking injections at the same site or maintain a gap of at least one day.
Maintain a diet that includes chapatis, puffed rice with vegetables, multigrain bread, plain cooked dal, roasted grams soups, sprouts, cooked vegetables with less oil, steamed vegetables, orange, jamun, guava, watermelon, apple, papaya, curd, cow’s milk, thin buttermilk, fish (baked, grilled, or steamed), cashew nuts, peanuts, and walnuts (handful). Avoid alcohol consumption and quit smoking. Exercise regularly and brisk walk daily for 30 minutes. Also, limit intake of sugar.
The risk factors for developing low blood sugar levels include not taking adequate meals or skipping meals, excessive insulin use, too much alcohol intake, fever and too much exercise. Some medications, like other diabetes medicine glimepiride, medicines used for fever and pain (salicylates), ramipril, etc., can result in such episodes when used with insulin. Inform your doctor about these episodes as you may need dose adjustment.
You are recommended to be extra cautious if you are about to take Insulin Glulisine with pioglitazone as Pioglitazone may cause fluid retention in your body, particularly when used along with insulin. You may develop heart failure symptoms such as swelling of hands and feet, edema, weight gain, breathlessness, etc. Also if you already have heart failure, it could worsen. Thus, please consult your doctor first before taking Insulin Glulisine with other medicines.
Insulin Glulisine contains a fast-acting insulin. Injecting Insulin Glulisine into a muscle would accelerate its absorption and increase the risk of serious episode of hypoglycemia (low blood sugar). Therefore, you should inject Insulin Glulisine just beneath the skin by pinching up some skin and fat.
Yes, you need to be careful about symptoms of hypoglycaemia (low blood sugar) such as increased heart rate may not be recognized by you. Thus, monitor your blood sugar regularly and consult your doctor if the problem persists.
It depends on whether you have type 1 diabetes mellitus or type 2. For patients with type 1, the only treatment available is external source of insulin which cannot be stopped, as your body does not produce adequate insulin. However, for patients with type 2 diabetes mellitus, the doctor may stop Insulin Glulisine if your blood sugar levels are well controlled with healthy diet, exercise and other diabetic medications. However, do not stop taking it on your own without consulting your doctor as it may worsen your condition.
Yes, Insulin Glulisine can cause hypoglycemia (low blood sugar levels). The symptoms include hunger, dizziness, sweating, nausea, irritability, headache, fast heart rate and feeling anxious or shaky. It occurs more frequently if you skip or delay meals, over-exercise, drink alcohol, or take other antidiabetic medicine along with it. So, it is important to regularly monitor blood sugar level. Always carry some sugary candies, fruit juice, glucose, or glucon-D with you.
Insulin Glulisine belongs to the class of antidiabetic drugs. It is a man-made form of insulin which is prescribed in diabetic adults and children of age 1 year and above. It helps improve blood sugar levels and glycemic control.